Extra Ventricular Device guideline (EVD)
exp date isn't null, but text field is
Scope
This guideline is intended for all healthcare professionals caring for patients with an EVD in the Paediatric Critical Care Unit at the Royal Hospital for Children, Glasgow.
Audience
All medical, nursing and allied professionals caring for patients who have an EVD should be familiar with the protocol.
Definition
External Ventricular Drains (EVDs) are a temporary system which allow drainage of cerebrospinal fluid (CSF) from the lateral ventricles of the brain.
EVDs are commonly used within neurosurgery for the management of patients who require drainage of CSF.
The EVD system is a closed system; breakage of the system would increase risk of contamination. Strict asepsis must be maintained.
Indications
Common indications include raised intracranial pressure (ICP) associated with:
- Head injury
- Subarachnoid haemorrhage
- Acute hydrocephalus
- Posterior fossa tumours
- Meningitis
Ventricular System Anatomy
There are four ventricles which comprise the ventricular system within the brain. The two lateral ventricles are the largest of the four, and are situated deep within the subcortical tissue, one each side of the midline. Each lateral ventricle communicates with the third ventricle through intra-ventricular foramina (Foramen of Monro). This third ventricle communicates with the fourth ventricle (located in the medulla) through the aqueduct of Sylvius (see Fig 1).
There are two lateral foramina and one median foramina located in the roof of the fourth ventricle which communicate with the subarachnoid space beneath the arachnoid membrane. The floor of the fourth ventricle is continuous with the central spinal canal.

Flow of CSF
The function of CSF is to provide buoyancy and support for the brain and spinal cord. It is a modified form of plasma consisting of water, glucose, protein, minerals and a few lymphocytes.
CSF is continuously secreted by the choroids plexus of the two lateral ventricles at a rate of approx. 20-25ml/hr (or 500ml/day).
At any one time, approx. 100-150ml of CSF are contained within the cerebral ventricles and the spinal cord. Once produced, it flows through the intraventricular foramen of Monro into the third ventricle and then through the single aqueduct of Sylvius into the fourth ventricle.
Once in the fourth ventricle, the CSF then flows into the subarachnoid space to flow around and over the brain, and into the spinal canal to flow around the spinal cord.
CSF is reabsorbed into the vascular circulation through the arachnoid villi at the saggital sinus. In health, the rate of reabsorbtion equals the rate of secretion.
An obstruction at any point in the flow of CSF will result in dilation of the cerebral ventricles and create a condition known as obstructive hydrocephalus. See Fig 2.
Failure of absorption of CSF at the saggital sinus will have the same effect on the ventricles but is known as communicating hydrocephalus.

Effects of CSF on Intracranial Pressure (ICP)
The Monro-Kellie hypothesis states that the skull is a rigid compartment filled to capacity with essentially incompressible substances (brain matter, blood and CSF). As such, an increase in one or more of the components will result in an increase in the overall pressure within the skull unless another component decreases in volume reciprocally.
ICP is thus affected directly by any changes in the volume of CSF within the brain. These changes in volume may be a result of –
- Change in the rate of secretion of CSF.
- Obstruction to the CSF flow within the ventricular system.
- Change in the rate of absorption of CSF.
Problems associated with the production, flow or absorption of CSF can cause a rise in ICP and therefore would be an indication for insertion of an EVD.

The above graph describes the relationship between pressure and volume within the skull. As can be seen, a reasonable increase in volume (irrespective of whether this is oedema, mass, blood or CSF) will be tolerated prior to ICP rising. The key is to intervene prior to reaching the critical point. Clinically this is associated with bradycardiac, hypertension and pupil changes. This is a pre-terminal event.
Infants:
- Irritability
- Vomiting
- Full, bulging fontanelle
- Neurological symptoms – decrease in GCS, cranial nerve palsy, sun-setting eyes (unable to look up)
- Irregular respirations & apnoeic periods
- Splaying of cranial sutures, a big head – measure head circumference regularly
- Tachycardiac /Hypertension /Bradycardia
- Pupil changes (fixed pupils, irregularly shaped pupils or dilated pupils all worrying)
Older children:
- Headache
- Nausea, vomiting
- Lethargy
- Irritability
- Worsening concentration
- Decreased GCS
- 6th nerve palsy
- Other abnormalities – seen at neurologic exam
- Tachycardiac /Hypertension/ Bradycardia
- Pupil changes (fixed pupils, irregularly shaped pupils or dilated pupils all worrying)
The combination of bradycardia, hypertension and irregular respiration in a neurological patient is a pre-terminal event. Inform medical staff IMMEDIATELY.
EVDs are inserted by a Neurosurgeon in the Operating Theatre under sterile conditions.
The catheter is then connected to the drainage system and the incision site on the scalp either sutured or stapled. Staples also secure the catheter to the scalp. Mark as an event on CIS when return from theatre.
*N.B. Untied purse string suture at the entry/exit site, identifiable with steri-strips at the end, is purposely left long to be tied off when EVD catheter removed. These should NOT BE CUT.
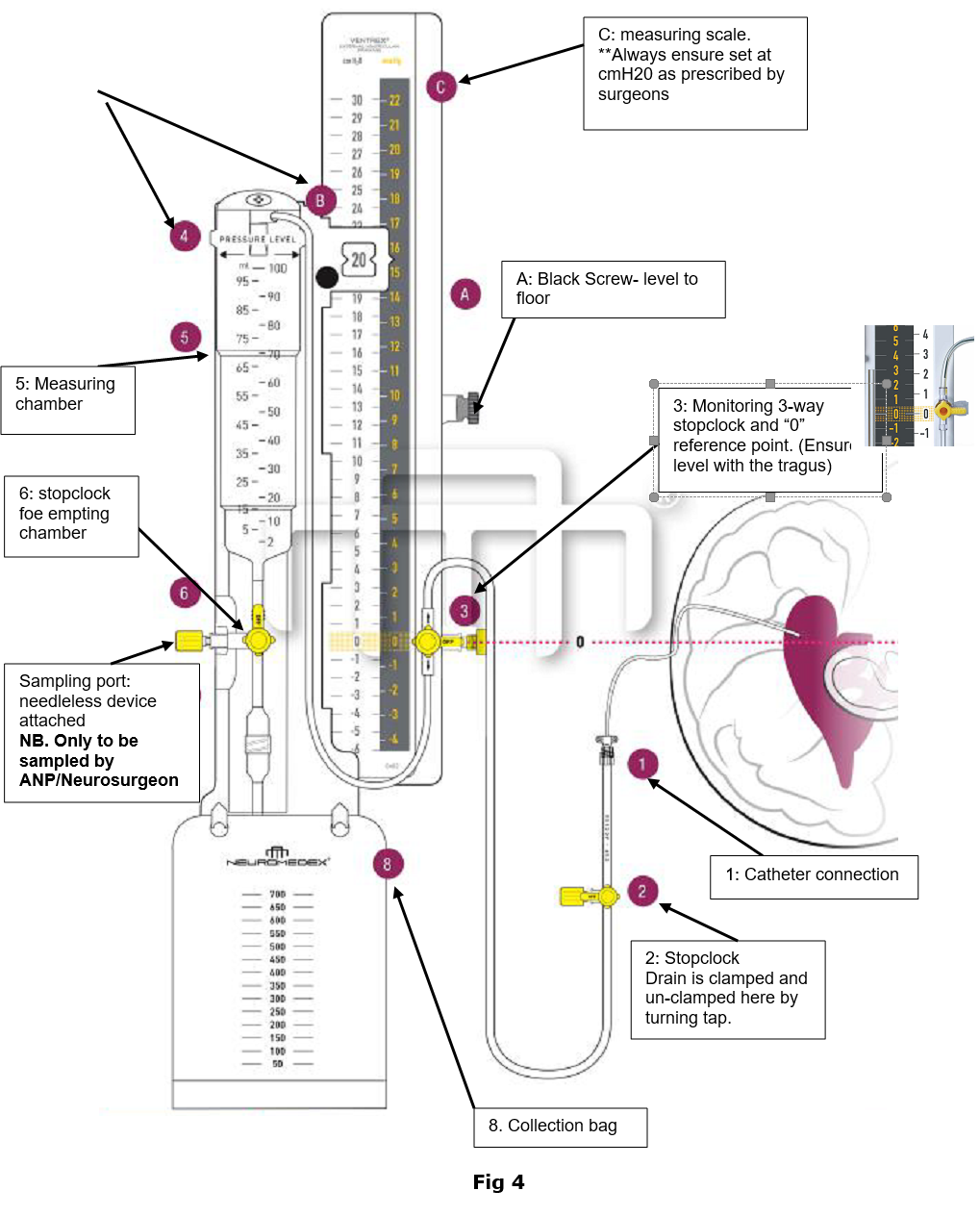
Once the EVD has been inserted, the surgeon attaches a VentrEx Complete EVD-System (Fig 3). (Fig 3). This is a complete closed system for draining CSF from the lateral ventricles in the brain. VentrEx Complete EVD-System does not have a pressure valve, so the drainage of CSF is gravity-dependent.
The drainage system is attached to an IV stand at the head of the bed.

Fig 3. VentrEx Complete EVD-System
The system comprises of a measuring chamber which is connected to a drainage bag, with a sampling port and stopcock between them. All the connections are “Luer-Lock” for safety.
A drainage pressure scale (in 1cm increments) is adjacent to the drainage chamber. The chamber should be zero referenced to the patient, aligned to the patient’s external auditory meatus (this corresponds with the Foramen of Monro). A Medtronic levelling clamp is used for. A Neurosurgeon will document the prescribed drain level, and be responsible for all subsequent alterations. (Fig 4.). The drain height will be displayed on a sign above the drain
NB: NRFitTM connectors for intrathecal and epidural procedures will be introduced as part of a National Patient Safety introduction therefore the VentrEx EVD system will be changing in the near future Within RHC to allow for NRFit connections. This guide will be update in accordance with this change.
Fig 4
Positioning, zeroing and securing
|
Procedure |
Rationale |
|
Maintain patient’s head elevation if |
To assist venous drainage of the head |
|
Maintain drainage system in vertical |
Ensure CSF drainage and avoid the air filter becoming wet which will lead to non-drainage. This can only be resolved by replacing the whole system. |
|
The zero reference point must be adhered to see Fig 4, number 3. |
The external auditory meatus should be taken as the reference point, as this is at the level of the foramen of Monro |
|
Slide chamber up the gauge until the arrow at the top of the chamber is at the height/level prescribed by neurosurgical staff, eg. 5cm The height/level should be displayed on the EVD sign which hangs above the drain.
Ensure the height/level of the drain is also documented on CIS. |
This means that the EVD is at 5cm above the foramen of Monro, and for CSF to drain, the CSF pressure within the ventricles must be at least 5cmH2O. This level will determine the amount of CSF drainage; for example, if the drain is set at 15cm and the ICP is less than 15cm H2O then there will be no drainage. If however the level/height is 15cm and the ICP is greater than 15cm H2O the system will drain to maintain the pressure ordered. Therefore if the drain is yielding 5-10ml/hr, the pressure inside the ventricles can be said to be 10-20cmH20, this is then a reflection of the ICP Monitor for clinical signs of high ICP as detailed above. |
|
Before moving the child for any reason (i.e sitting up or lying down) the drain must be clamped. Following the procedure, re-establish the zero point and unclamp the drain. The 3–way tap is used to clamp and unclamp. See Fig 4 |
Re-positioning could cause an over drainage of CSF. Ensure unclamp drain post procedure – otherwise ICP could climb quickly. |
|
The drainage system is positioned at the head of the bed/cot. If impossible to stretch beyond cot sides – the EVD must be put through the cot sides and NOT over the top. |
This will affect the level at which CSF is drained. |
|
The EVD system must be secured to a drip stand at the head of the bed, facing the foot of the bed. |
To ensure that accidental removal is avoided. |
|
The EVD system must be clearly labelled with the pink EVD stickers, preferably near the 3 way tap. |
To avoid confusion with other lines. |
|
Change the collection bag (using Universal Precautions) when ¾ full. See appendix A. |
Hourly observations
|
Procedure |
Rationale |
|
Observe the tubing for patency/kinked obstruction. Document on CIS |
If obstructed the patient may redevelop hydrocephalus. |
|
Ensure the CSF oscillates with respiration. Ensure the CSF drips into the chamber. Document on CIS
|
If there is no drainage, but the drain is patent, the meniscus of the CSF should be seen to swing because of pulsatile pressure. If the drainage is zero, and the CSF is not seen to swing, this could mean the drain is blocked. Inform medical team. |
|
Ensure that the tubing has not been clamped and that all the taps are in the open position. |
To allow CSF to drain and prevent hydrocephalus and raised ICP. |
| Record CSF drainage hourly (on CIS) and empty the amount of CSF drained. |
The amount of CSF drainage is an indication of the ICP. An increase could indicate mounting intracranial pressure. |
|
Replace ml/ml CSF losses with 0.9% Sodium Chloride or as instructed by the Neurosurgical Team. |
If large volumes of CSF are lost there is a greater risk of hyponatremia in patients, which could lead to potential seizers. Daily bloods (U+E’s) should be obtained for all patients with an EVD to check sodium levels. |
|
Report excessive drainage if the amount of drainage exceeds 10ml more than the previous hour or more than 20ml/hr, OR if cessation of drainage, to the consultant intensivist as a matter of urgency. |
Average drainage for an adult is 10-15ml/hr. Excessive drainage can collapse the ventricles, pulling brain from dura. This may lead to a subdural haematoma. |
|
Be vigilant with fluid balance and electrolytes, particularly if there are large losses or prolonged need for EVD. |
Particularly in small babies (<5kg). May need to replace volume. |
| Observe CSF for colour and consistency. Normal CSF is clear and colourless. Report if cloudy, milky, or turbid, yellow or newly red. |
Cloudy, milky or turbid CSF may equal infection. Yellow/orange CSF (xanthochromic) contains partially broken-down red blood cells from previous haemorrhage. Red –fresh blood, may indicate cerebral haemorrhage or recent surgery. |
|
Monitor the patient’s neurological responses and pupillary response. Report any significant changes to the consultant intensivist. Tentorial herniation can occur with over or under drainage – as well as deteriorating GCS, the patient may be irritable, have vital signs changes, and respiratory compromise if this occurs. Neurobservations should be performed more frequently if the drain has been raised or lowered recently or if clamped for Intrathecal (IT) antibiotics or transfer - this is patient dependent. 15 min neuro obs may be appropriate. |
To detect any deterioration in the patient’s condition, which may be a result of ICP. |
|
Record the fontanelle if present - Tense/Normal/Sunken |
Another marker of ICP. Alert medic if changes. |
|
Observe the insertion site for signs of infection. Report pyrexia to medical staff. |
As the catheter has direct passage into the brain, there is an increased risk of meningitis. There is a reported risk of infection of 1-27% with EVD’s. |
|
Report any CSF leakage from the insertion site to a Neurosurgeon. |
If the dressing appears wet at the entry site this could indicate CSF leak or may present as a halo stain on pillow. |
Infection
|
Procedure |
Rationale |
|
A strict aseptic technique must be used during any sampling or maintenance procedures. NB** Sampling of EVD will only be undertaken by ANP/Neurosurgical Registrar. |
As the catheter has direct passage into the brain, there is an increased risk of meningitis. There is an infection risk of 1-27% with EVD’s. |
|
Many of the EVD’s inserted will be impregnated with antibiotic. Eg. Bactiseal (rifampicin and clindamycin) |
To reduce levels of infection. |
|
In the presence of intracerebral infection, intraventricular antibiotics may be instilled (under strict aseptic technique) by the Neurosurgeon. After instillation, the drain will be clamped for one hour, to allow the antibiotic to circulate with the CSF. Increase neuro observations to every 30 mins during this time. |
Strict asepsis to reduce introduction of infection. Occasionally antibiotics are required to be instilled directly into CSF to ensure penetration. Ensure drain unclamped 1 hour post procedure. If patient changes clinically at any point during this time inform doctor immediately. |
|
CSF samples will be requested and obtained by the Neurosurgical Team and sent to Bacteriology (MC&S) and Biochemistry (protein & glucose) See photograph below. Normal <5WBC. WBC:RBC <1:500-1000 |
Could indicate that an infection is occurring whether that be meningitis or ventriculitis. |
Fig 6.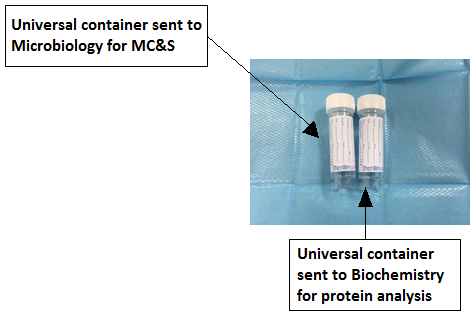
Transfer
A checklist is available on CIS and intranet for transfer of the child with an EVD in situ.
|
Procedure |
Rationale |
|
Before moving the child for any reason (i.e sitting up or lying down) the drain must be clamped. (do this by turning the stopclock 2 off 2 towards the patient). Following the procedure, re-establish the zero point and unclamp the drain (open the stopclock to the patient and “off” to the empty port). Fig. 4, number 2. Eg. If moving a patient from bed to trolley or onto CT scan, this process should be followed. |
Re-positioning could cause an over drainage of CSF. Ensure unclamp drain post procedure – otherwise ICP could climb quickly. |
|
When in transit: eg. in ambulance/ going to CT - aim to maintain CSF drainage during transfer. Once the patient is settled on the bed/trolley and the zero-point is re-established, the drain should be unclamped. The patient must be closely monitored to prevent accidental disconnection or any alteration in position, which may affect CSF drainage. The transfer trolley has a pole at the head of the bed which can be used to secure the drain. A pole must be attached securely to the hospital bed to maintain an upright EVD system. |
To ensure adequate CSF drainage and prevent rises in ICP.
To avoid accidental disconnection, ensure adequate CSF drainage.
|
|
A decision to clamp the EVD must be made following assessment of the patient's clinical condition and neurological status; it must be clamped for the briefest time possible. Re-open/unclamp the drain as soon as possible – during CT scan or once in transit. |
Clamping an EVD may result in inadequate CSF drainage and subsequent rise in ICP, however there are occasions when it may be necessary to clamp the system for short periods. |
Golden rules
- EVD tubing must not be irrigated, changed or manipulated in any way other than by a Neurosurgeon or trained delegate.
- If any concerns report to medical staff quickly. A decrease in pulse rate and an increase in BP or an alteration in consciousness may indicate a rise in ICP. An awake child may also complain of headaches if their ICP changes
Any changes must be reported immediately to medical staff
As with any invasive device, an EVD may become a source of infection.
Within this paediatric critical care unit, sampling is carried out on request of the Neurosurgeon on ward round.
**Sampling will ONLY BE OBTAINED by the Paediatric Neurosurgical ANP or the Neurosurgical Registrar.
The procedure is:
-
Assemble a clean dressing trolley with a dressing pack, sterile gloves, 10ml syringe, needleless smart site, and two white-topped, universal containers bottles (Fig. 6).
-
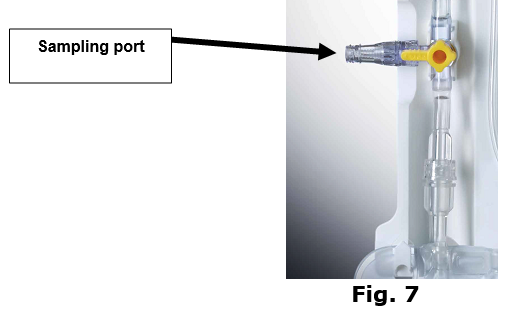
Ensure the sample port has a needless smart site attached, if not apply one.
-
Clean the sampling port beneath the collection chamber with a Chloraprep wipe, and allow to dry.
-
Don sterile gloves, attach 10ml syringe and withdraw specimen of CSF (2-3ml to each Lab as an ideal, but 0.5ml is the minimum required) (Fig. 6) - Remove syringe and add CSF sample equally to containers.
-
Send one to Bacteriology (for culture, sensitivity and cell count), and one to Biochemistry for protein analysis (Fig. 6) - Change needless smart site after sample obtained (Fig. 7).
The drain is removed (when no longer required) by a Neurosurgeon (or delegate), under strict aseptic technique. Often, removal is preceded by a period where the height of the drain has been increased, or the drain has been clamped (to see if the patient can regulate their own CSF again).
The surgeon will require a clean dressing trolley (Neuro trolley), set up with –
- Dressing pack
- Betadine or other (surgeon dependent)
- Sterile gloves
- Staple removers
- Stitch cutter
- Hand-held suture
- Sterile scissors
- White-topped universal container
- Primapore (or similar) dressing
It may be appropriate to increase neuro observations after removal of drain. Clarify with neurosurgeon (or delegate) removing drain.
It is possible, although not routine, to monitor intracranial pressure through the ventricular catheter using a continuous closed monitoring system with a non-flush transducer device. See separate guideline: Measuring ICP from an EVD.
The collection bag must be changed:
a) When ¾ full
b) Under strict aseptic non touch technique (ANTT)
c) Only by a trained member of staff
The procedure:
- Put on apron
- Wash hands and trolley
- Prepare equipment.
- Turn 3 way clamp off to patient. Consider goggles.
- Wash hands, sterile towel to dry hands. Don sterile gloves.
- Using a strict aseptic technique clean bag connector/tubing with chloraprep and allow to dry for 30 seconds.
- Remove bag and attach bung to seal contents.
- Reattach new bag.
- Reopen 3 way tap.
- Check that fluid is pulsating within tubing.
- Clear away and wash hands.
If at any time accidental disconnection should occur, the ventricular catheter should immediately be clamped and the patient nursed in a supine position until the catheter is reconnected using aseptic technique.
If it is thought that the ventricular catheter or the EVD system has become contaminated, or indeed it cannot be guaranteed that they have not, then a neurosurgeon must be contacted immediately as it may be necessary to change the entire system.
Accidental cutting or splitting of tubing will lead to a free flow of CSF. The catheter should be clamped immediately with atraumatic forceps (blue forceps) Fig 8. and the neurosurgeon informed.
Despite best nursing care, EVD’s may be dislodged completely, particularly in the awake and active child. Cover site with a sterile dressing from safety pack, Fig 9. Inform neurosurgeon.

NOTE: an Extra Ventricular Drainage system troubleshooting guide & EVD Safety Pack are available in Appendix 1 & 2.
The management of a lumbar drain is fairly similar to that of an EVD, seek specific guidance from neurosurgery.
The zero-point is level with the top of the mattress. Patient lying flat on back.
The level is often set at 0 or 5cmH2O.
Sampling is the same process as for an EVD – see above.
The indications for insertion include; assist healing of CSF leak, evaluate the effect of reducing CSF pressure, and as a temporary external shunt.
|
DISCONNECTION OF EVD FROM SYSTEM |
|
1. CLAMP VENTRICULAR CATHETER OR SHUT 3 WAY TAP (if possible wrap end of the EVD in a betadine swab) |
|
2. NURSE PATIENT IN SUPINE POSITION 3. CONTACT NEUROSURGEONS |
|
4. RECONNECT CATHETER USING ASEPTIC TECHNIQUE or Prime new EVD drain |
|
5. FAST PATIENT UNTIL A DECISION IS MADE |
|
*NOTE – NOTE – IF IT IS THOUGHT THE VENTRICULAR CATHETER OR SYSTEM HAS BECOME CONTAMINATED, NEUROSURGEONS MUST BE MADE AWARE OF THIS AS THE WHOLE SYSTEM MAY REQUIRE TO BE CHANGED |
|
CUTTING OR SPLITTING OF VENTRICULAR CATHETER |
|
1.CLAMP IMMEDIATELY WITH ATRAUMATIC FORCEPS (BLUE FORCEPS) |
|
2.INFORM NEUROSURGEONS IMMEDIATELY |
|
3.IF ANY CSF LEAKAGE COVER AREA WITH STERILE DRESSING |
|
4.FAST THE PATIENT UNTIL A DECISION HAS BEEN MADE |
|
ACCIDENTAL REMOVAL OF VENTRICULAR CATHETER |
|
1.COVER AREA IMMEDIATELY WITH STERILE GAUZE AND APPLY LIGHT PRESSURE |
|
2.APPLY STERILE DRESSING |
|
3.INFORM NEUROSURGEON IMMEDIATELY |
|
4.FAST THE PATIENT UNTIL A DECISION HAS BEEN MADE |
** AT EACH STAGE IT IS IMPORTANT TO REMEMBER THAT THE PATIENT MAY BE EITHER LOSING OR HAVE A BUILD OF CSF. THE PATIENT SHOULD BE MONITORED CLOSELY FOR ANY SIGNS OF DECREASED CONSCIOUS LEVEL.
NEUROLOGICAL OBSERVATIONS SHOULD BE CARRIED OUT MORE FREQUENTLY DURING THIS TIME. ANY CHANGE IN GCS SHOULD TO BE REPORTED TO MEDICAL STAFF, WHO WILL CONTACT NEUROSURGEONS.
EQUIPMENT REQUIRED:
- Blue forceps/clamps (atraumatic clamps)
- Sterile swabs
- Sterile dressing
- Cleaning agent (clinell wipes)
- Skin cleansing agent (chloraprep)

- EVD Guideline Alder Hey 2010.
- EVD Guideline Birmingham 2009.
- EVD Guideline Leeds 2009.
- EVD Guideline – Neurosurgical Institute Glasgow -2011
- Woodward, S. Benchmarking Best Practice for External Ventricular Drainage. Br J of Nursing 2002: 11(1); 47-53.
Permission obtained from Delta Surgical to use images and resources for VentrEx Complete EVD-System.
Last reviewed: 17 December 2024
Next review: 31 December 2027
Author(s): S Forsyth, L Todd, J Grady, J Brown, E Campbell, L Moore
Approved By: PICU Guideline Group
Reviewer Name(s): L Moore, H Gavin, A McGettrick, E Campbell, L Todd