Management of neutropenia & fever: antibiotic policy
exp date isn't null, but text field is
Objectives
Management of neutropenia with a fever, including an antibiotic, anti-viral and anti-fungal policy for this group of patients.
Scope
Children with neutropenia and fever, especially children with haematological and/ oncology conditions.
Neutropenia is defined as a neutrophil count of <1 x 109/L and patients who are neutropenic are vulnerable to overwhelming infection. The frequency and severity of infective episodes correlates with the degree and duration of neutropenia and is particularly marked in children whose neutrophil count is below 0.5 x 109/l.
This guideline should be read in conjunction with the assessment, diagnosis and management of Neutropenic Sepsis, Best Practice Statement, publication date: September 2012 (see Section 6.1).
3.1 The diagnosis and management of febrile neutropenia will be directed by the Consultant/Associate Specialist or a senior member of the medical team.
3.2 The Medical/Nursing team will be responsible for admitting, assessing, investigating and administrating treatment, and monitoring response.
None.
Criteria for Treatment
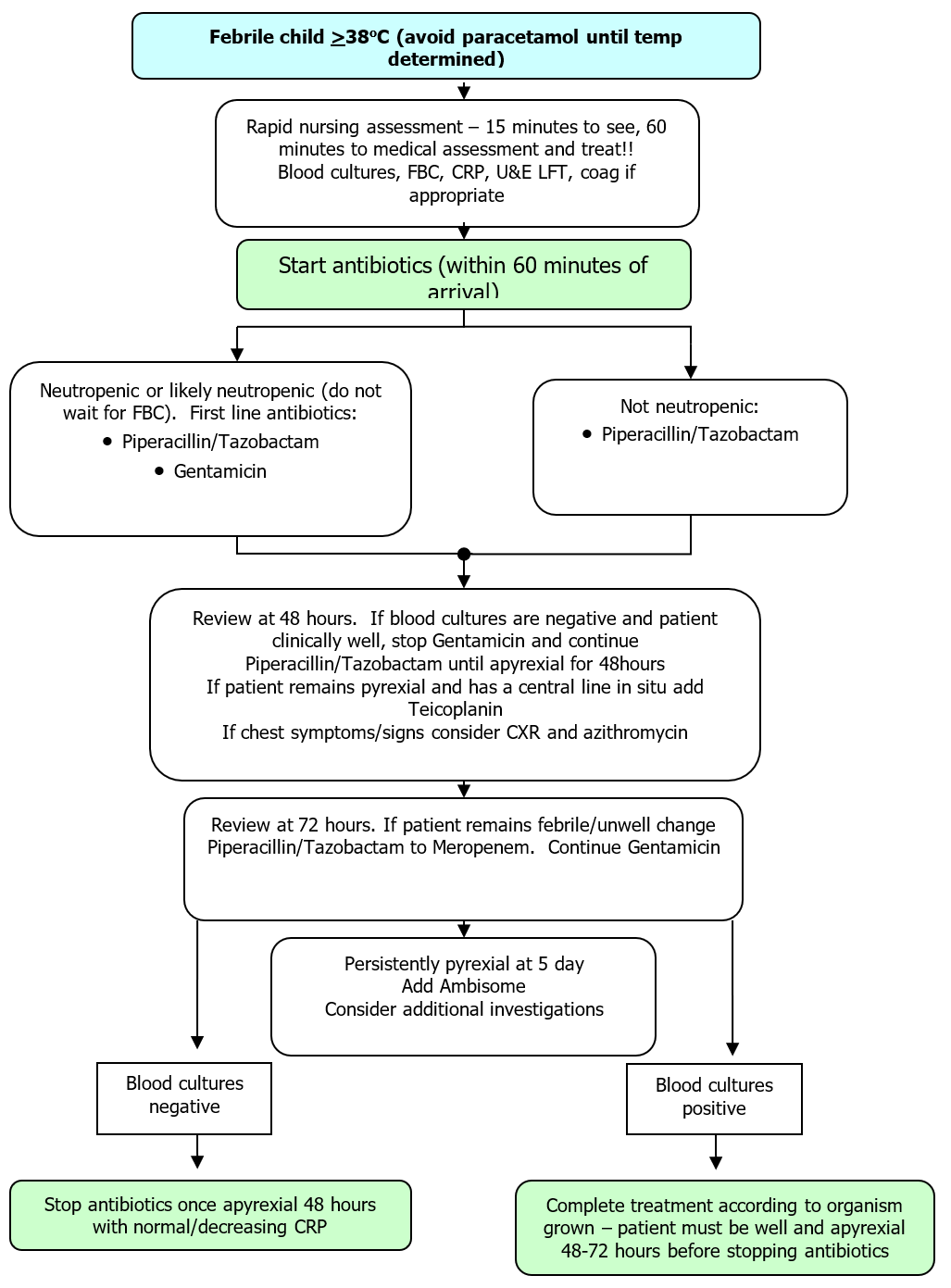
- Any child with a single temperature of >38oC should receive intravenous antibiotics (in line with the national policy).
- Paracetamol should not be given until the decision to treat has been taken because it may mask a fever. Particular care should be exercised with HSCT patients who are neutropenic.
- Any child who deteriorates, looks unwell or rigors regardless of his/her temperature and neutrophil count should receive intravenous antibiotics. Fever may be suppressed by steroids, particularly Dexamethasone, and these children may become septic and deteriorate rapidly without exhibiting fever.
- It is always better to over rather than under treat these patients. These children can deteriorate rapidly.
IN A NEUTROPENIC PATIENT, THE OCCURRENCE OF FEVER MUST BE REGARDED AS AN EMERGENCY
- The initial nursing assessment of the patient must happen within 15 minutes of the patient’s arrival. Medical assessment and administration of antibiotics must happen within 60 minutes from the patient’s arrival.
- An 'ill' child must be assessed immediately even in the absence of a fever. A DELAY IN ADMINISTERING THE FIRST DOSE OF ANTIBIOTICS MAY PROVE FATAL – and antibiotic administration must not be delayed for any reason (including shift changes, ward rounds, radiological examination, problems with venous access). Blood cultures should be taken before giving the first dose of antibiotics.
!!!! The first dose of antibiotics can precipitate septic shock
!!!!! Be prepared to resuscitate the patient
- Patients who are unwell or hypotensive should immediately receive resuscitation fluids and IV antibiotics, even if they are not pyrexial. Remember steroids can mask an inflammatory response.
- If a patient deteriorates after using/flushing his/her central line consideration should be given to siting a peripheral cannula and stopping using the line.
- All haematology/oncology patients admitted overnight who are ill, must be seen by the most experienced middle grade doctor on for hospital cover who should discuss the patient causing concern with the consultant haematologist/oncologist on-call.
History and Examination
- Keep the history brief. The following will help predict the likely degree and duration of neutropenia and identify a potential focus that might guide antibiotic therapy. Note:
- The diagnosis
- The date and type of the last chemotherapy given
- Any recent blood counts
- The duration of fever
- The presence of a central line (NB line associated sepsis)
- The presence of bleeding
- Any muscle, joint or abdominal pain
- The presence of mucositis
- Any local cause for fever
- Examination: Ask yourself:
- Does the child require resuscitation?
- Is the child septicaemic or shocked?
- What is the temperature, HR, RR, BP, oxygen saturation and Capillary Refill Time (CRT)
- Is there an obvious focus for infection?
Investigations
- Blood cultures (take a large volume)
- FBC and differential
- CRP
- U&Es
- LFTs and Coagulation screen: PT, APTT, Fibrinogen +/- d-dimers if unwell – not every child requires a coagulation screen
- Urine sample if child is <5 years
- Consider a CXR if respiratory signs or symptoms (this must not delay therapy)
- If upper respiratory symptoms are present, consider NPA, viral throat swab
Treatment
- Resuscitate the child
- Give empirical IV antibiotics within 1 hour
- Give blood products as indicated
Microbiological Cultures
Blood Cultures:
- Blood cultures should be taken from the central line prior to IV antibiotic administration, or where there is no central line, from a peripheral sample.
- The volume required is 5 - 10 mls or a minimum of 3-5 mls from an infant. In the case of a double lumen long line, or two separate central lines, blood cultures should be taken from each lumen.
- Blood cultures should be repeated in the event of:
- Clinical deterioration
- Rigors
- Persistent pyrexia after 24 and 48 hours and thereafter 48-72 hourly if the patient remains pyrexial
- Prior to any antibiotic change
- Recurrence of fever after period of apyrexia
- If blood cultures are initially positive, repeat cultures should be taken after 48 hrs to confirm the organism has been eradicated (in vitro sensitivities do not always correlate with in vivo sensitivity).
- In the case of a central line infection, which is often due to bacterial growth in a biofilm, it is advisable to repeat line cultures after stopping antibiotics to check that the organism has been eradicated.
Additional investigations should be performed:
- Swab of central line exit site(s)
- Consider:
- Viral serology or culture / PCR if symptoms are suggestive of viral infection
- Nose swab
- Throat swab
- Sputum culture
- Urine culture
- Stool culture
- Swabs of any lesion or potential focus
- A chest X-ray may be indicated. Remember that in pneumocystits carinii pneumonia the chest may be clear to auscultation when there is hypoxia and marked radiological change.
(see appendix 2 for antibiotic dosing advice)
First Line Antimicrobial Therapy
- Suspected/Confirmed Neutropenic Patients
First line empirical therapy in neutropenic patients is with Piperacillin/Tazobactam and Gentamicin in the absence of positive blood cultures which would indicate alternative antibiotics. Piperacillin/Tazobactam is a penicillin based antibiotic and penicillin allergy should be excluded. Patients known to be colonised with ESBL producing organisms should receive Meropenem.
- Prescribe Piperacillin/Tazobactam according to pharmacy dose banding chart.
- Gentamicin requires caution in patients at risk of renal impairment. However, it is extremely unlikely that one single dose of Gentamicin will do harm and a single dose should be given and levels measured before any subsequent doses.
- Patients initially started on Piperacillin/Tazobactam and Gentamicin can stop Gentamicin if subsequently shown not to be neutropenic and they are neither septic or shocked.
- NB Piperacillin increases the risk of toxicity when given with Methotrexate. For any patient imminently due IV Methotrexate at any dose >500mg/m2 or who is post IV Methotrexate and has not cleared to acceptable levels, prescribe Meropenem as first line empirical therapy.
- Antibiotic cover for line-related infection:
- Teicoplanin should be added to the initial therapy only if there is a proven or a very high suspicion of central line infection. Teicoplanin is preferable to vancomycin for patients receiving other nephrotoxic drugs and most haemato/oncology patients are on other nephrotoxic drugs. Factors suggesting line infection include:
- Local Sepsis: Erythema at exit site or skin tunnel; pain over tunnel or on moving that arm/shoulder
- Previously documented catheter related sepsis involving the current central venous line
- Rigor or fever after flushing line (within 4 hours)
- Blood culture positive for an organism associated with the related infection
Vancomycin, rather than Teicoplanin should only be used in patients suspected to have a line related infection and who are septicaemic.
Second Line Antimicrobial Therapy
- Patients who remain pyrexial after 72 hours of empirical therapy should change to second line therapy. Second line therapy is with Meropenem with or without Gentamicin.
- Patients who remain pyrexial at 5 days and who are or have been persistently neutropenic with no evidence of line related infection should have AmBisome This should be discussed with the consultant responsible for the care of the patient.
Penicillin Allergy
- Serious allergy is one that causes an anaphylactic or urticarial reaction. 10% of patients with reactions to penicillin-based antibiotics will also have a reaction with cephalosporins.
- Patients who have had an allergic reaction classified as serious should receive Ciprofloxacin & Vancomycin.
- If ciprofloxacin has been given as prophylaxis, discuss treatment with Consultant Microbiologist on call.
Duration of Antimicrobial Treatment
This depends on the degree and duration of neutropenia and the organism cultured, but as a general rule:
- Patients who are blood culture negative; stop antibiotics after 48 hours of apyrexia if the patient is well and if the blood cultures are negative.
- Patients who are culture positive: this depends on the organism and the degree and duration of neutropenia. Discuss the duration of antibiotics with microbiology/ID. Preferably repeat blood cultures should be documented to have no growth.
- Gentamicin should not be given for more than 7 days. If the child needs additional gram negative non-aminoglycoside antimicrobial cover, discuss with the microbiologist.
- First line therapy for patients who are known not to be neutropenic or expected not to be neutropenic, and considered low risk for developing severe sepsis, should be single agent Piperacillin/Tazobactam.
- Patients started on both Piperacillin/Tazobactam and Gentamicin should stop the aminoglycoside if subsequently found not to be neutropenic, if neither septic nor shocked.
Antipyrexial Treatment
Once cultures have been taken and antibiotics started it is acceptable to treat the fever with Paracetamol. Do not give non-steroidal anti-inflammatories such as ibuprofen. Non-steroidals are contraindicated because of their effect on platelet function.
Chemotherapy
Withhold oral chemotherapy for Acute Leukaemia patients. Refer to individual treatment protocol /guidelines for other haemato/oncology patients to establish if chemotherapy should be stopped temporarily in the neutropenic patient. Note: In certain protocols, chemotherapy is continued even in the presence of neutropenic fever. Discuss with consultant.
Examination
The child should be examined daily for signs of infection including sites such as the mouth, axillae, ears, perineum and central catheter site.
Co-trimoxazole as PCP Prophylaxis
Continue co-trimoxazole prophylaxis whilst other antibiotics are being given unless the patient is receiving high dose co-trimoxazole intravenously or consultant thinks that co-trimoxazole should be temporarily discontinued to allow count recovery. Prophylaxis need not be given intravenously but can be temporarily withheld in patients who are nil by mouth.
This SOP will be reviewed in 24 months time.
None
NB Antibiotic doses in this guideline are appropriate for empirical treatment or sensitive organisms only. For any organism categorised as ‘I’ (Susceptible – increased exposure), seek further advice or refer to local policy for appropriate dose selection’ (see NHS GGC Clinical Guidelines Portal)
- Assessment, Diagnosis and Management of Neutropenic Sepsis - Best Practice Statement (publication date: September 2012) - www.gov.scot (put “neutropenic sepsis” into the search engine).
- BNF – access via bnf.nice.org.uk
- BNF for Children – access via bnfc.nice.org.uk
- www.renaldrugdatabase.com
- NHSGGC Clinical Guidelines Portal
- Guidelines for the management of paediatric line-related sepsis
Last reviewed: 01 August 2024
Next review: 31 August 2026
Author(s): J Sastry
Version: 6
Approved By: Sch Clin Gov Group
Document Id: HAEM-ONC-003